From previous posts we now know that chemo-sensitive and chemo-resistant clones compete even when space is abundant and thus sensitive cells can be used to control the resistant population. We also know that in many, probably most cases, chemotherapy alone will not kill a tumour and that just “giving it all we got” is likely to expedite the emergence of resistant untreatable tumours. So, are Adaptive Therapies (ATs) so much better?
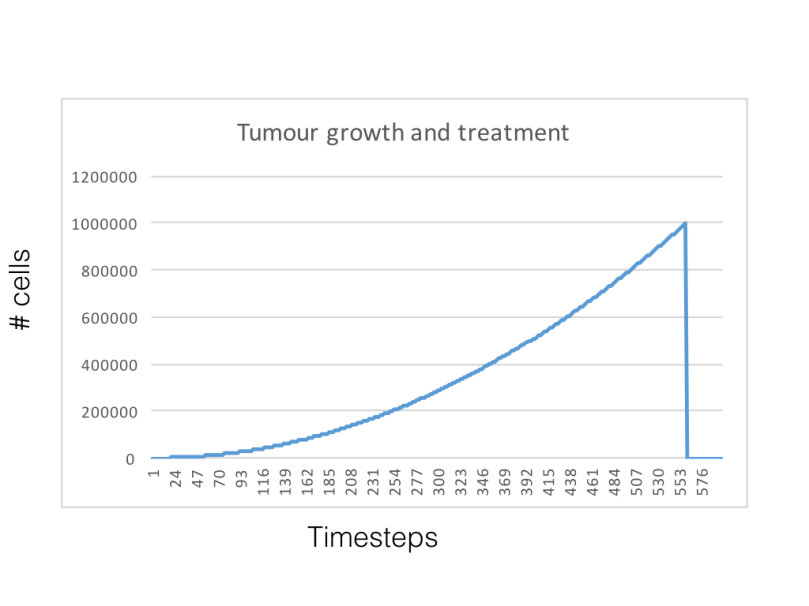
I have read a few slightly different implementations of ATs by the authors (CR 2009, Biol Direct 2010, CR 2012). The easiest definition of an AT involves the use of chemotherapy only as a way to control a population. Thus we will define a population size we want to achieve and some margin around which we can allow some wiggle. So let’s compare three simulations, one with no treatment, one with conventional lets-give-it-all chemo and one with an AT. The AT will aim to control the tumour population around the 100,000 cells mark and cease chemo when the population goes below 90,000. Here’s a simulation that shows how the AT approach works in this implementation:
As it is before, darker colors represent susceptible cells but as the cells display brighter colors (cyan->yellow->red) they become less susceptible.
And this plot compares the change in tumour population for the three different simulations (untreated, conventional chemo and AT):

The results show that not treating the tumor is clearly the worst of the options, that using chemotherapy in a conventional way can quickly select for resistance and that ATs could be a worthwhile alternative. The little insert on the top-left corner shows what happens when we run AT for longer. The Untreated and conventional treatments were run for about half the time that AT was, mostly because I could see what the result would be at the end. The effects of AT clearly do not last for ever and, if you look at the movie, it is easy to see why: every time the treatment is applied the overall phenotypic composition of the tumor shifts slightly towards more resistance.
Of course this has only scratched the surface of the issue. A more systematic and thorough comparison would allow us not only to be more certain about the advantages of ATs over conventional application of chemotherapy but also to say something about the importance of intra tumour heterogeneity in determining this.
Interestingly, mathematical models of AT typically assume resistance to be binary: either the cell is resistant (in which case it will resist any amount of chemo) or is not. I decided to try to see how AT would work on a version of the model where cells are either resistant or susceptible. I think the results suggest that AT would work better under this binary assumption which makes me think that ATs would work even better in treatments where evolution would have a less smooth landscape to operate on.
It is clear to many of us that ATs (and other evolutionary enlightened approaches such as evolutionary double binds) are likely to be more effective in many situations. The NCI has invested some good money to further explore this idea. Even a clinical trial is currently under way at Moffitt to test approaches based on AT in prostate cancer. But as we said on the first post of this series, the trade off is that we would need to consider cancer as a chronic disease and not something that could be cured once and for all. This would seem a reasonable compromise for a lot of patients but if we could find out more about which ones would do better with AT and which ones we can treat in a more definite way , that would be undoubtedly better. I expect that tumour heterogeneity (its origin and the mechanisms that maintain it) and a better understanding of the interactions with the microenvironment will be key for help us determine this. Expect some more thorough analysis discussing these points in a preprint server near you .