I am currently in a small city in Germany: Bielefeld, as a guest of the Center for Interdisciplinary Research (ZiF in German) of the University of Bielefeld. During this time I will be working with other ZiF fellows on a couple of projects which I hope to discuss some other time. This work will be within the framework of a ZiF cooperation group called Multiscale Modeling of Tumor Initiation, Growth and Progression.
To kick start this, the organizers of this cooperation group have also organized a small workshop on mathematical modelling of cancer evolution. This being exactly the topic of my research for the last decade meant I was really excited to participate. The image at the top of this post shows many (but not all) of the participants.
Any interdisciplinary meeting will include people from at least two disciplines with the goal of the meeting being to establish some sort of bridge between them. In this case I could argue that the disciplines were mathematicians working on less applied topics vs those working on more applied ones (or biologists as one of them referred to us).
But where I stand, the more interesting gap to bridge was between those interested on the genetic aspects of cancer evolution and those (me and Indiana’s James Glazier) which focused instead on the role of selection. If you ask me (and by reading these lines you have implicitly done so) both genetic variation and selection are the two pillars of evolution and should be considered equally important. Nonetheless there seems to be a lot more work done in trying to understand genetic mutations and phylogenetic trees than in trying to see how the microenvironment and interactions between different cells determines which phenotypes will succeed and which ones will not. More importantly, selection is a key aspect of evolution that we need to understand if we want to have any success when applying treatments to anything from cancer to bacteria to viruses. Why are they (apparently) vastly more people working on genetic aspects rather than selection?

I think that this difference between workflows might partly explain why. There is a wealth of biological data, much of which is genetic in nature, which requires a comparatively modest degree of collaboration with experimentalists if you are a modeler. The process is described in the previous figure: use a mathematical model to find out what the data tells you and then generate hypotheses out of it.
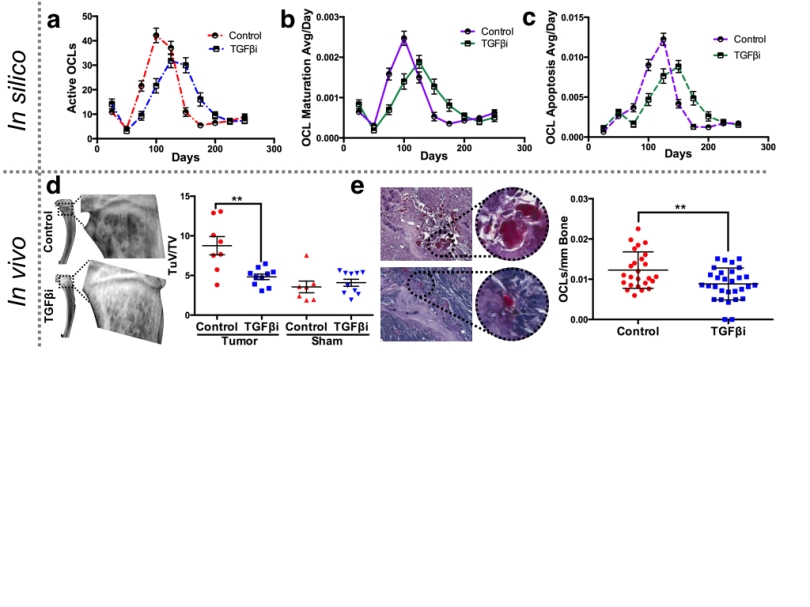
Working on selection requires a different approach as there’s not much data available, especially data that could be easily slotted in a mechanistic model of cancer evolution. Here the mathematical model, built after much consultation with domain experts (that is, cancer biologists) is built to explore the biology and yield hypotheses, which, since we involved our experimental partners from the start, will be also explored in vivo or in vitro. This route is harder but also relatively unexplored, want to join?